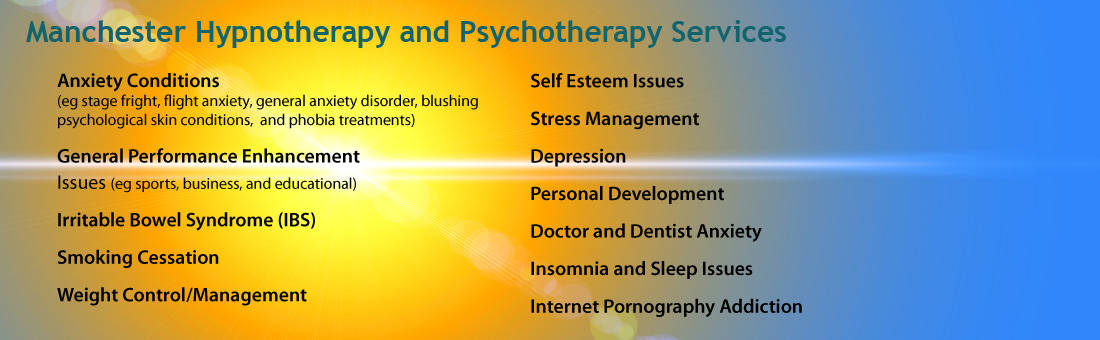
Hypnotherapy for Phobia and Anxiety Manchester

Anxiety Treatment Manchester
Many people now seek anxiety treatment Manchester. Panic attacks, anxiety and phobia, extreme shyness, obsessive-compulsive behaviours, and generalized anxiety disrupt the lives of an estimated 15% of the population. Anxiety is part of normal human experience. We all know what it feels like to be anxious; it can be a beneficial experience as it can help us to prepare for something or take more care than we otherwise might, but for some people,these moments of anxiety aren’t isolated and rare like they are for most people. Instead, anxiety is a constant and dominating force that severely disrupts the quality and enjoyment of their lives and goes far beyond mere occasional”nervousness.” Hypnotherapy and Hypno-Psychotherapy are very effective for anxiety treatment Manchester.
Let’s look at the different types of anxiety that I work with:
PANIC DISORDER: Panic disorder manifests itself in unexpected or unpredictable attacks of extreme anxiety, with symptoms including rapid heartbeat, shortness of breath, trembling,sweating, nausea and dizziness. Some may have chest pain or smothering sensations, and/or a sense of unreality. Hands may tingle or feel numb, and some feel flushed or chilled. Some victims feel they are losing their minds or are about to die. They have a fear of impending doom or loss of control. Many become so obsessively worried about subsequent attacks that they make major changes in their behaviours, shunning whatever situation may have prompted the panic. People with panic disorder have feelings of terror that strike suddenly and repeatedly with no warning. They can’t predict when an attack will occur, and many develop intense anxiety between episodes, worrying when and where the next one will strike. In between times there is a persistent, lingering worry that another attack could come any minute. Attacks can occur any time, even during non dream sleep. While most attacks average a couple of minutes, occasionally they can go on for up to 10 minutes. In rare cases, they may last an hour or more.
Panic Attack Symptoms– Pounding heart– Chest pains– Light-headedness or dizziness– Nausea or stomach problems– Flushes or chills– Shortness of breath or a feeling of smothering or choking– Tingling or numbness– Shaking or trembling– Feelings of unreality– Terror– A feeling of being out of control or going crazy– Fear of dying– Sweating Panic disorder strikes at least 1.6 percent of the population and is twice as common in women as in men. It can appear at any age–in children or in the elderly–but most often it begins in young adults. Not everyone who experiences a panic attack will develop panic disorder– for example, many people have one attack but never have another. For those who do have panic disorder, though, it’s important to seek treatment. Untreated, the disorder can become very disabling. Panic disorder is often accompanied by other conditions such as depression or alcoholism, and may spawn phobias, which can develop in places or situations where panic attacks have occurred. For example, if a panic attack strikes while you’re riding an elevator, you may develop a fear of elevators and perhaps start avoiding them. Some people’s lives become greatly restricted–they avoid normal, everyday activities such as shopping, driving, or in some cases even leaving the house. Or,they may be able to confront a feared situation only if accompanied by a spouse or other trusted person. Basically, they avoid any situation they fear would make them feel helpless if a panic attack occurs. When people’s lives become so restricted by the disorder, as happens in about one-third of all people with panic disorder, the condition is called agoraphobia. A tendency toward panic disorder and agoraphobia runs in families. Nevertheless, early treatment of panic disorder can often stop the progression to agoraphobia.Here are some examples of how it feels to have Panic Disorder:
“Before I had anxiety treatment Manchester it started 10 years ago. I was sitting in a seminar in a hotel and this thing came out of the clear blue. I felt like I was dying.” “For me, a panic attack is almost a violent experience. I feel like I’m going insane. It makes me feel like I’m losing control in a very extreme way. My heart pounds really hard, things seem unreal, and there’s this very strong feeling of impending doom.” “In between attacks there is this dread and anxiety that it’s going to happen again. It can be very debilitating, trying to escape those feelings of panic.”
AGORAPHOBIA: Agoraphobia typically results from the fear of having a panic attack in specific situations “from which escape might be difficult (or embarrassing) or in which help may not be available in the event of having an unexpected or situationally predisposed Panic Attack or panic-like symptoms” (DSMV-IV). Literally, “fear of open spaces or of being in crowded, public places like markets” from the ancient Greek agora or market, agoraphobia is generally understood as fear manifested in the avoidance of a cluster of situations such as crowded places, heights, being alone, being in a crowd or standing in a line; being on a bridge; and travelling in a bus, train, or car. Agoraphobia can lead to extreme anxiety and avoidance,leading some victims to become “housebound,” unable to leave a very small “safe-zone.” The early treatment of anxiety helps avoid the escalation of symptoms into agoraphobic behaviour. Agoraphobia is responsive to both therapeutic and medical anxiety treatment Manchester.
GENERALISED ANXIETY DISORDER: Generalized anxiety disorder (GAD) is much more than the normal anxiety people experience day to day. It’s chronic and exaggerated worry and tension, even though nothing seems to provoke it. Having this disorder means always anticipating disaster, often worrying excessively about health, money, family, or work. Sometimes, though, the source of the worry is hard to pinpoint. Simply the thought of getting through the day provokes anxiety.People with GAD can’t seem to shake their concerns, even though they usually realize that their anxiety is more intense than the situation warrants. People with GAD also seem unable to relax. They often have trouble falling or staying asleep.Their worries are accompanied by physical symptoms, especially trembling,twitching, muscle tension, headaches, irritability, sweating, or hot flashes. They may feel light headed or out of breath. They may feel nauseated or have to go to the bathroom frequently. Or they might feel as though they have a lump in the throat.Many individuals with GAD startle more easily than other people. They tend to feel tired, have trouble concentrating, and sometimes suffer depression, too. Depression often accompanies anxiety disorders and, when it does, it needs to be treated as well. The feelings of sadness, apathy, or hopelessness, changes in appetite or sleep, and difficulty concentrating that often characterize depression can be effectively treated.Usually the impairment associated with GAD is mild and people with the disorder don’t feel too restricted in social settings or on the job. Unlike many other anxiety disorders, people with GAD don’t characteristically avoid certain situations as a result of their disorder. However, if severe, GAD can be very debilitating, making it difficult to carry out even the most ordinary daily activities.GAD comes on gradually and most often hits people in childhood or adolescence, but can begin in adulthood, too. It’s more common in women than in men and often occurs in relatives of affected persons. It’s diagnosed when someone spends at least 6 months worried excessively about a number of everyday problems.In general, the symptoms of GAD seem to diminish with age.
Here are some examples of how it feels to have GAD: “I always thought I was just a worrier. I’d feel keyed up and unable to relax. At times it would come and go, and at times it would be constant. It could go on for days.I’d worry about what I was going to fix for a dinner party, or what would be a great present for somebody. I just couldn’t let something go.” “I’d have terrible sleeping problems. There were times I’d wake up wired in the morning or in the middle of the night. I had trouble concentrating, even reading the newspaper or a novel. Sometimes I’d feel a little light headed. My heart would race or pound. And that would make me worry more.”
SPECIFIC PHOBIA: Many people experience specific phobias, intense, irrational fears of certain things or situations–dogs, closed-in places, heights, escalators, tunnels, driving,water, flying, and injuries involving blood are a few of the more common ones.Phobias aren’t just extreme fears; they are irrational fears. You may be able to ski the world’s tallest mountains with ease but panic going above the 10th floor of an office building. Adults with phobias realize their fears are irrational, but often facing, or even thinking about facing, the feared object or situation brings on a panic attack or severe anxiety. Specific phobias strike more than 1 in 10 people. They seem to run in families and are a little more prevalent in women. Phobias usually first appear in adolescence or adulthood. They start suddenly and tend to be more persistent than childhood phobias; only about 20 percent of adult phobias vanish on their own. When children have specific phobias–for example, a fear of animals–those fears usually disappear over time, though they may continue into adulthood. No one knows why they hang on in some people and disappear in others.If the object of the fear is easy to avoid, people with phobias may not feel the need to seek treatment. Sometimes, though, they may make important career or personal decisions to avoid a phobic situation.
Here are some examples of how it feels to have a Specific Phobia: “I’m scared to death of flying, and I never do it any more. It’s an awful feeling when that air plane door closes and I feel trapped. My heart pounds and I sweat bullets.If somebody starts talking to me, I get very stiff and preoccupied. When the air plane starts to ascend, it just reinforces that feeling that I can’t get out. I picture myself losing control, freaking out, climbing the walls, but of course I never do. I’m not afraid of crashing or hitting turbulence. It’s just that feeling of being trapped.Whenever I’ve thought about changing jobs, I’ve had to think, “Would I be under pressure to fly?” These days I only go places where I can drive or take a train. My friends always point out that I couldn’t get off a train travelling at high speeds either, so why don’t trains bother me? I just tell them it isn’t a rational fear.” “Just the thought of coming into direct contact with a dog keeps me out of the park. Walking along a street is ok as dogs are on leads and I can cross to the other side. If a dog comes up to me though, I panic and am likely to lash out! That doesn’t make me very popular!” “I was driven over the Severn Bridge last week. I had to lie down on the back seat as I felt so faint. I was sweating and crying. I wanted to run away and scream!”
SOCIAL ANXIETY: Social Anxiety disorder (also known as social phobia) is generally understood as extreme fear in the face (or anticipation) of social interaction. While social anxiety disorder is poorly understood, researchers are beginning to focus on this disorder that is experienced by as many as 7 % of the population at any one time. Social Anxiety is not mere shyness, but a medically recognized disorder that severely hampers the quality of life. It is estimated that between 7 and 13% of people are affected by social anxiety disorder at some point, making social anxiety the third largest mental health disorder as identified by the DSM-IV. Simply put, Social Anxiety Disorder is understood as being the recurring avoidance and debilitating fear of social situations where one might possibly be negatively be judged by others. Socially anxious people typically experience uncomfortable emotional and physical distress when they: ⢠are thrust into the centre of attention ⢠are teased ⢠introduced to strangers ⢠have to speak or perform before an audience ⢠are being watched while doing something physical ⢠are talking with an “important” person ⢠exchange eye contact ⢠eat, drink, or speak in the presence of others ⢠enter any unfamiliar social situation Labels and Symptoms: Because people with social phobia are easily embarrassed and insecure in social interactions, they are commonly labelled as being “shy,” “timid,” “uptight,” and even”rude,” and “aloof.” These perceptions tend to exacerbate the situation for the social phobic, increasing the already intense anxiety of the situation by adding to it the nearly self-fulfilling anticipation of negative judgement by others.Unfortunately, these labels also complicate the diagnostic process by confusing a potentially treatable disorder with the expectation that such behaviour is the result of innate and simple personality traits. What distinguishes social anxiety from the common but occasional fear of embarrassment is the chronic nature of the disorder. Certain social situations (specific phobia) or nearly all social situations(generalized anxiety) are persistently accompanied by feelings of dread,worthlessness, negative thoughts, increased heart rate, weak knees, twitching muscles, blushing, trembling limbs, dry mouth, and/or constant anxiety. These physical and emotional symptoms are also usually understood by the person with social anxiety as being irrational in nature, but impossible to avoid.
Here are some examples of how it feels to have a Social Phobia: “I couldn’t go on dates or to parties. For a while, I couldn’t even go to class. During my second year of college I had to come home for a semester.” “My fear would happen in any social situation. I would be anxious before I even left the house, and it would escalate as I got closer to class, a party, or whatever. I would feel sick to my stomach–it almost felt like I had the flu. My heart would pound, my palms would get sweaty, and I would get this feeling of being removed from myself and from everybody else.” “When I would walk into a room full of people, I’d turn red and it would feel like everybody’s eyes were on me. I was too embarrassed to stand off in a corner by myself, but I couldn’t think of anything to say to anybody. I felt so clumsy, I couldn’t wait to get out.”
Social phobia often begins around early adolescence or even younger. If you suffer from social phobia, you tend to think that other people are very competent in public and that you are not. Small mistakes you make may seem to you much more exaggerated than they really are. Blushing may seem painfully embarrassing,and you feel as though all eyes are focused on you. You may be afraid of being with people other than those closest to you. Or your fear may be more specific,such as feeling anxious about giving a speech, talking to a boss or other authority figure, or dating. The most common social phobia is a fear of public speaking. Sometimes social phobia involves a general fear of social situations such as parties. More rarely it may involve a fear of using a public toilet, eating out, talking on the phone, or writing in the presence of other people, such as when signing a cheque. Although this disorder is often thought of as shyness, the two are not the same. Shy people can be very uneasy around others, but they don’t experience the extreme anxiety in anticipating a social situation, and they don’t necessarily avoid circumstances that make them feel self-conscious. In contrast, people with social phobia aren’t necessarily shy at all. They can be completely at ease with people most of the time, but particular situations, such as walking down an aisle in public or making a speech, can give them intense anxiety. Social phobia disrupts normal life, interfering with career or social relationships. For example, a worker can turn down a job promotion because he can’t give public presentations. The dread of asocial event can begin weeks in advance, and symptoms can be quite debilitating.
OBSESSIVE-COMPULSIVE DISORDER:Obsessive-compulsive disorder is characterized by anxious thoughts or rituals you feel you can’t control. If you have OCD, as it’s called, you may be plagued by persistent, unwelcome thoughts or images, or by the urgent need to engage in certain rituals.You may be obsessed with germs or dirt, so you wash your hands over and over.You may be filled with doubt and feel the need to check things repeatedly. You might be preoccupied by thoughts of violence and fear that you will harm people close to you. You may spend long periods of time touching things or counting; you may be preoccupied by order or symmetry; you may have persistent thoughts of performing sexual acts that are repugnant to you; or you may be troubled by thoughts that are against your religious beliefs.The disturbing thoughts or images are called obsessions, and the rituals that are performed to try to prevent or dispel them are called compulsions. There is no pleasure in carrying out the rituals you are drawn to, only temporary relief from the discomfort caused by the obsession.A lot of healthy people can identify with having some of the symptoms of OCD,such as checking the stove several times before leaving the house. But the disorder is diagnosed only when such activities consume at least an hour a day,are very distressing, and interfere with daily life.Most adults with this condition recognize that what they’re doing is senseless, but they can’t stop it. Some people, though, particularly children with OCD, may not realize that their behaviour is out of the ordinary.OCD strikes men and women in approximately equal numbers and afflicts roughly 1 in 50 people. It can appear in childhood, adolescence, or adulthood, but on the average it first shows up in the teens or early adulthood. A third of adults with OCD experienced their first symptoms as children. The course of the disease is variable–symptoms may come and go, they may ease over time, or they can grow progressively worse. Evidence suggests that OCD might run in families. Depression or other anxiety disorders may accompany OCD. And some people with OCD have eating disorders. In addition, they may avoid situations in which they might have to confront their obsessions. Or they may try unsuccessfully to use alcohol or drugs to calm themselves. If OCD grows severe enough, it can keep someone from holding down a job or from carrying out normal responsibilities at home, but more often it doesn’t develop to those extremes.
Here are some examples of how it feels to have OCD: “I couldn’t do anything without rituals. They transcended every aspect of my life. Counting was big for me. When I set my alarm at night, I had to set it to a number that wouldn’t add up to a “bad” number. If my sister was 33 and I was 24, I couldn’t leave the TV on Channel 33 or 24. I would wash my hair three times as opposed to once because three was a good luck number and one wasn’t. It took me longer to read because I’d count the lines in a paragraph. If I was writing a term paper, I couldn’t have a certain number of words on a line if it added up to a bad number.I was always worried that if I didn’t do something, my parents were going to die. O rI would worry about harming my parents, which was completely irrational. I couldn’t wear anything that said Boston because my parents were from Boston. I couldn’t write the word “death” because I was worried that something bad would happen.” “Getting dressed in the morning was tough because I had a routine, and if I deviated from that routine, I’d have to get dressed again. I knew the rituals didn’t make sense, but I couldn’t seem to overcome them until I had therapy.” “I thought about sex all the time. But I never enjoyed sex, and I didn’t like the thoughts. I just couldn’t do anything to stop myself.”
POST-TRAUMATIC STRESS DISORDER: Post-Traumatic Stress Disorder (PTSD) is a debilitating condition that follows a terrifying event. Often, people with PTSD have persistent frightening thoughts and memories of their ordeal and feel emotionally numb, especially with people they were once close to. PTSD, once referred to as shell shock or battle fatigue, was first brought to public attention by war veterans, but it can result from any number of traumatic incidents. These include kidnapping, serious accidents such as car or train crashes, natural disasters such as floods or earthquakes, violent attacks such as a mugging, rape, or torture, or being held captive. The event that triggers it may be something that threatened the person’s life or the life of someone close to him or her. Or it could be something witnessed, such as mass destruction after a plane crash.Whatever the source of the problem, some people with PTSD repeatedly relive the trauma in the form of nightmares and disturbing recollections during the day. They may also experience sleep problems, depression, feeling detached or numb, or being easily startled. They may lose interest in things they used to enjoy and have trouble feeling affectionate. They may feel irritable, more aggressive than before,or even violent. Seeing things that remind them of the incident may be very distressing, which could lead them to avoid certain places or situations that bring back those memories. Anniversaries of the event are often very difficult. PTSD can occur at any age, including childhood. The disorder can be accompanied by depression, substance abuse, or anxiety. Symptoms may be mild or severe–people may become easily irritated or have violent outbursts. In severe cases they may have trouble working or socializing. In general, the symptoms seem to be worse if the event that triggered them was initiated by a person, such as a rape, as opposed to a flood.Ordinary events can serve as reminders of the trauma and trigger flashbacks or intrusive images. A flashback may make the person lose touch with reality and re-enact the event for a period of seconds or hours or, very rarely, days. A person having a flashback, which can come in the form of images, sounds, smells, or feelings, usually believes that the traumatic event is happening all over again.Not every traumatized person gets full-blown PTSD, or experiences PTSD at all. PTSD is diagnosed only if the symptoms last more than a month. In those who do have PTSD, symptoms usually begin within 3 months of the trauma, and the course of the illness varies. Some people recover within 6 months, others have symptoms that last much longer. In some cases, the condition may be chronic. Occasionally, the illness doesn’t show up until years after the traumatic event.
Here is an example of how it feels to have PTSD: “I was raped when I was 25 years old. For a long time, I spoke about the rape on an intellectual level, as though it was something that happened to someone else. I was very aware that it had happened to me, but there just was no feeling. I kind of skidded along for a while. I started having flashbacks. They kind of came over me like a splash of water. I would be terrified. Suddenly I was reliving the rape. Every instant was startling. I felt like my entire head was moving a bit, shaking, but that wasn’t so at all. I would get very flushed or a very dry mouth and my breathing changed. I was held in suspension. I wasn’t aware of the cushion on the chair that Iwas sitting in or that my arm was touching a piece of furniture. I was in a bubble,just kind of floating. And it was scary. Having a flashback can wring you out. You’re really shaken. The rape happened the week before Christmas, and I feel like a werewolf around the anniversary date. I can’t believe the transformation into anxiety and fear.”
CO-EXISTING CONDITIONS: Many people have a single anxiety disorder and nothing else, but it isn’t unusual for an anxiety disorder to be accompanied by another illness, such as depression,an eating disorder, alcoholism, drug abuse, or another anxiety disorder. Oftenpeople who have panic disorder or social phobia, for example, also experiencethe intense sadness and hopelessness associated with depression or become dependent on alcohol. In such cases, these problems will need to be treated as well.
It should be noted that hypnotherapy treatment for anxiety and phobia is evidenced based.
Brookhouse Hypnotherapy Manchester has been helping people just like you to make significant improvements with phobia and anxiety issues in order to live a happier and more fulfilling life. If you would like more information, please contact me at enquiries@hypnomanchester.co.uk or call 0161 881 1677 for an appointment for phobia and anxiety treatment Manchester.




 Brookhouse Hypnotherapy
Brookhouse Hypnotherapy